What is Parotid Gland?
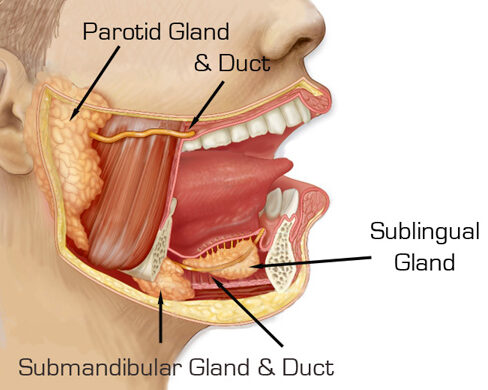
The parotid gland is the largest of the salivary glands located in the human body. It is situated below the cheekbone, and in front of the ear. Each person has two parotid glands, one on each side of the face.
The parotid gland plays a crucial role in the production and secretion of saliva, which helps in the initial digestion of food. Saliva contains enzymes that break down food particles, making it easier to swallow and digest. The parotid gland produces a watery type of saliva that is rich in enzymes called amylase, which aids in the digestion of starches and carbohydrates.
The gland has a duct known as Stensen’s duct, which opens into the mouth at the level of the upper molars. This duct allows saliva to flow from the parotid gland into the oral cavity.
The parotid gland can be affected by various conditions, including infections, tumors, and inflammation. In some cases, parotid gland tumors may develop, which can be either benign (noncancerous) or malignant (cancerous).
Why do I need parotid surgery?
Parotid surgery, also known as parotidectomy, is a surgical procedure performed on the parotid gland. There are several reasons why someone may need parotid surgery, including
1. Tumors: The most common indication for parotid surgery is the presence of tumors in the parotid gland. These tumors can be either benign or malignant. Benign tumors, such as pleomorphic adenomas, are usually removed to prevent growth, compression of nearby structures, or the risk of transformation into malignancy. Malignant tumors, such as mucoepidermoid carcinoma or adenoid cystic carcinoma, may require surgical removal to treat the cancer and prevent its spread.
2. Infections: Severe or recurrent infections of the parotid gland, such as recurrent parotitis, may necessitate surgical intervention. In some cases, the ducts that carry saliva from the gland to the mouth can become blocked or obstructed, leading to recurrent infections. Surgery can help remove the obstruction and improve salivary flow.
3. Salivary Stones: Salivary stones, also known as sialolithiasis, can develop within the salivary glands, including the parotid gland. These stones can cause pain, swelling, and infection. Parotid surgery may be required to remove the stone and relieve the associated symptoms.
4. Chronic Inflammation: Chronic inflammation of the parotid gland, such as in chronic recurrent parotitis, can cause persistent pain, swelling, and recurrent infections. Surgical treatment may be considered when conservative measures, such as antibiotics or gland massage, fail to provide relief.
5. Facial Nerve Disorders: The facial nerve, which controls the muscles of facial expression, passes through the parotid gland. In certain conditions, such as facial nerve tumors or severe trauma, surgery may be necessary to address the nerve disorder while preserving its function.
It’s important to note that the decision to undergo parotid surgery is made after a thorough evaluation by a medical professional. They will assess the specific condition and determine the most appropriate treatment plan, which may involve surgical intervention.
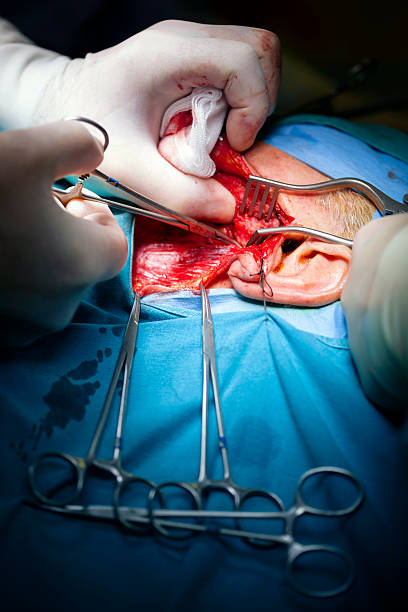
What does Parotid Surgery entail?
Parotid surgery, also known as parotidectomy, is a surgical procedure performed to remove part of the parotid gland.(commonly) or whole of the gland (less commmonly). The procedure is performed under general anesthesia, meaning you will be unconscious during the surgery. The surgeon will make an incision in front of or slightly below the ear, along natural skin creases to minimize visible scarring. The size and location of the incision may vary depending on the specific reason for the surgery. During the procedure, the surgeon carefully identifies and isolates the facial nerve, which passes through the parotid gland. Preserving the facial nerve function is crucial to avoid complications such as facial weakness or paralysis.Surgeon may use nerve monitor (special equipment) to help in identification and preservation of facial nerve. The surgeon then removes the affected portion of the parotid gland, which may involve removing tumours, infected areas, or other problematic structures.
After removing the necessary tissue, the surgeon may close the incision with stitches or surgical staples. In some cases, a drain may be placed near the surgical site to remove any excess fluid or blood during the initial healing phase. Following the surgery, you will be monitored in a recovery area until the effects of the anesthesia wear off. Pain medication may be prescribed to manage any discomfort, and you may be advised to follow specific post-operative care instructions, such as keeping the surgical area clean and avoiding strenuous activities for a certain period. Recovery time can vary depending on the extent of the surgery and the individual’s healing process. It’s essential to attend follow-up appointments with your surgeon to monitor healing, remove any stitches, and assess the overall outcome of the procedure. It’s important to consult with a qualified healthcare professional to discuss your specific situation, potential risks, benefits, and expected outcomes of parotid surgery. They will be able to provide personalised guidance and address any concerns you may have.
What are the risks/ complications of surgery?
Like any surgical procedure, parotid surgery carries potential risks and complications. It’s important to have a detailed discussion with your surgeon before the procedure to understand the specific risks and potential complications in your case. They will be able to provide you with personalized information based on your medical history and individual circumstances. While the majority of parotid surgeries are successful, it’s important to be aware of the possible risks involved. These risks can include:
1. Facial Nerve Injury: The facial nerve runs through the parotid gland, and during surgery, it is crucial to identify and protect this nerve. However, there is a small risk of inadvertent damage to the facial nerve, which can lead to temporary or permanent facial weakness, asymmetry, or even paralysis. Surgeons take great care to minimize this risk, and specialised techniques, such as nerve monitoring, may be employed to enhance nerve preservation.
2. Frey’s Syndrome: Frey’s syndrome, also known as gustatory sweating, is a condition that can occur after parotid surgery. It involves abnormal sweating and flushing on the cheek or neck while eating or thinking about food. It happens due to the misdirection of nerve fibers that control sweating in the area. Although it is generally not a serious concern, it can be bothersome for some individuals.
3. Sialocoele: saliva can leak into the surrounding tissues, forming a fluid-filled cavity known as a sialocele. The accumulation of saliva can cause swelling, pain, and discomfort in the affected area. In some cases, the sialocele may resolve on its own as the damaged duct or gland heals. However, persistent or symptomatic sialoceles may require treatment. Treatment options for sialoceles may include: Conservative Management: In some cases, smaller sialoceles may be managed conservatively with measures such as applying warm compresses, gentle massage, and the administration of pain relievers. This approach allows time for the damaged duct or gland to heal and for the sialocele to resolve spontaneously. Aspiration and Compression: Larger or persistent sialoceles may require aspiration, which involves draining the accumulated saliva using a needle and syringe. After aspiration, compression may be applied to help close the disrupted duct or gland and prevent further leakage. Surgical Intervention: If conservative measures and aspiration do not provide sufficient relief or if the sialocele recurs, surgical intervention may be necessary. The specific surgical technique will depend on the location and extent of the sialocele but generally involves identifying and repairing the damaged duct or gland. In some cases, the surgeon may need to remove a portion of the affected gland or create a diversion for saliva flow.
4. Salivary Fistula: Occasionally, after parotid surgery, a connection or abnormal passage called a salivary fistula can develop between the remaining salivary gland tissue and the skin surface. This can result in saliva leakage through the incision or wound. Most cases of salivary fistula resolve spontaneously, but in some cases, additional treatment or intervention may be required.
5. Infection: As with any surgical procedure, there is a risk of infection at the surgical site. It’s important to follow proper wound care instructions to prevent infection and seek medical attention if any signs of infection, such as increased pain, redness, swelling, or fever, occur.
6. Bleeding or Hematoma: There is a risk of bleeding during or after surgery, which can lead to the formation of a hematoma (a collection of blood). In some cases, additional surgery may be necessary to control bleeding or remove a haematoma.
7. First bite syndrome (FBS) is a rare condition characterized by severe pain in the parotid region during the initial bite or first few bites of a meal. It typically occurs following surgery in the parotid gland or in the vicinity of the gland, such as parotidectomy or neck dissection procedures. FBS is thought to be related to nerve damage or irritation in the region. The exact cause of FBS is not fully understood, but it is believed to be associated with injury or stretching of the branches of the auriculotemporal nerve, a nerve that supplies sensation to the parotid gland and the surrounding area. During surgery, the nerve may be inadvertently damaged or affected, leading to the development of FBS. Symptoms of first bite syndrome can include severe pain on the affected side of the face or jaw, specifically when the person takes the first few bites of a meal. The pain is typically described as sharp, stabbing, or burning in nature and may last for several minutes after eating. Management of first bite syndrome focuses on relieving symptoms and improving quality of life. Treatment options for FBS may include: Medications like Nonsteroidal anti-inflammatory drugs (NSAIDs) or neuropathic pain killers, Dietary Modifications, Nerve Block Injections, Botulinum Toxin Injections (Botox). Time and Symptom Management: In many cases, first bite syndrome improves over time as the nerves heal. Learning strategies to manage the pain, such as taking smaller bites, eating slowly, and using heat or cold therapy, can help individuals cope with the symptoms.
8. Scar Formation: Although surgeons attempt to make incisions in discreet locations to minimize scarring, some degree of scarring is inevitable. The appearance of the scar will vary from person to person and can be influenced by factors such as skin type and the individual’s healing ability.
9. Other General Risks: General risks associated with any surgery, such as adverse reactions to anesthesia, blood clots, or allergic reactions to medications, are possible but relatively rare.

Leave a Reply